On June 25, 2021, I attended a webinar hosted by CRE-MSD, presented by Dr. Nick LaDelfa which he called, “Neuromuscular response to repetitive workloads relative to current upper extremity ergonomics thresholds”. That sounds a bit intimidating, but I’ll try to make it more practical for you here.
Over the past year or so, we’ve been using La Delfa’s arm strength research, combined with Dr. Jim Potvin’s fatigue equations, and University of Michigan’s biomechanical model, in almost every project we’ve touched. I was eager to hear La Delfa’s thoughts and to see if our approach needed to change.
A key concept relies on understanding the research definition of fatigue: a decrease in strength. Your strength is as good as it gets when you start fresh…perhaps you can lift 100 lbs at the beginning of the day! At the end of a tiring day, if we asked you to lift your maximum again, you might cap out at 90 lbs. The goal in designing work “ergonomically” is to ensure that, when leaving the workplace at the end of the day, workers have the same strength as they started with. We also want them to have same great productivity and quality outputs in the last hour of the shift as the first.
The gold standard of “fatigue as a decrease in strength” means that you must measure strength to determine if someone is fatigued. And exerting strength so it can be measured CAUSES fatigue. A dilemma indeed. We obviously can’t go around fatiguing workers at the beginning and end of each shift.
Many methods aim to measure or predict fatigue, often using workers’ estimates of effort or pain; you may have heard of the Borg Scale, for example, which uses a 10-point scale. Employee exertion-rating is an area of research that LaDelfa discussed in his presentation. In our practice, we tend to avoid using exertion ratings, partly because the person we see doing the job on assessment day may be stronger than the person we need to assess for. Researchers have also used electromyography (a.k.a. EMG), which measures the electrical signals in your muscles; the signals from your muscles change when the muscles become tired. But this method, while still used in a research setting, hasn’t been very practical in the field.
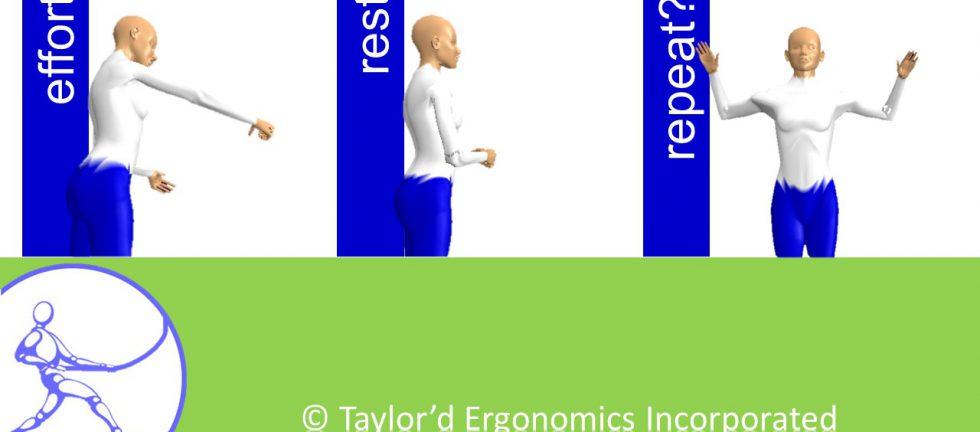
However, that lab research has been very useful at predicting when a muscle will fatigue. We know, for example, that if you exert a really heavy effort, you’ll need a certain amount of rest before you have your full strength back. And if you exert a really light effort for a long time, you’ll also need a specific, predictable amount of rest before you’re ready to go again. These effort/rest ratios form the basis of the best ergonomics analysis tools that are currently available. In the US, the ACGIH (American Conference of Governmental Industrial Hygienists) publishes guidelines for a variety of hazards (physical, amongst many others). They promote the “duty cycle” method, which is similar to the one we use. LaDelfa’s research suggests that Potvin’s Maximum Acceptable Effort (MAE) method protects workers from fatigue even more effectively than ACGIH’s model. Good – our “in-the-field” process continues to align with the most current research available.
Many other ergonomics assessment tools exist, and most are easier to use than the MAE method; you may have heard of Liberty Mutual tables (which we do use when they are appropriate), the NIOSH equation, RULA, and strain index. Why would we go to the trouble of using a biomechanical model and a calculation, if we could use a checklist tool to advise that a task needs to be imrpoved? What does the MAE do that these tools can’t do?
- The MAE can be used to assess postures that the basic tools have not incorporated, such as one-handed pushing, holding efforts for long periods, sideways pushing, or repetitive, awkward bending with light weights.
- The MAE, with a biomechanical model, can allow us to estimate the effect of leaning on an object.
- But what our clients appreciate most is that it allows us to do better “what if” analyses. When you want to choose the best solution for a problem, the MAE allows you to account for small changes in the amount of force, task frequency, reach, hand height, the direction of force, and more. With the simpler tools, you might suggest a lift table that would allow the worker to raise or lower a load, but the change might not be sufficient to show any improvement in risk at all. You might reduce the force required to install a part from 10 kg to 3 kg, and RULA might still suggest that the task is high risk. The more sensitive MAE can demonstrate the effect of even a small change.
Is the MAE more work than the older methods? Yup. But that’s what we’re trained for.